Understanding Non Hormonal Birth Control: Methods, Benefits, and Considerations
Reclaiming Control,Naturally.
For many individuals, the journey to finding the right birth control method is a deeply personal one, often fraught with decisions balancing efficacy, convenience, and potential side effects. While hormonal contraception has long dominated the landscape, offering high effectiveness and various benefits beyond pregnancy prevention, it’s not a universal fit. Concerns about hormonal fluctuations, mood changes, weight gain, or simply a desire to live more in tune with one’s natural body rhythms have led to a growing interest in alternatives. This is where non hormonal birth control steps in, offering a compelling array of options for those seeking effective pregnancy prevention without the influence of synthetic hormones.
Imagine a world where you have reliable control over your reproductive health, yet remain entirely free from the systemic effects of hormones. This isn’t a distant dream; it’s a reality accessible through a diverse range of non-hormonal methods. From age-old barrier techniques perfected for modern use to sophisticated devices and knowledge-based strategies, non-hormonal contraception provides a powerful pathway to reproductive autonomy.
This comprehensive guide will unveil the world of non-hormonal birth control, exploring its various forms, their mechanisms of action, effectiveness rates, and what makes each option unique. We’ll delve into the benefits and considerations, empowering you with the knowledge to make an informed decision that aligns with your health philosophy and lifestyle. Whether you’re experiencing side effects from hormonal methods, planning for future pregnancy, or simply prefer a natural approach, understanding non-hormonal birth control is your first step towards reclaiming control, naturally.
The Copper IUD –Highly Effective and Hormone-Free LARC
In the quest for effective, long-term, and hormone-free contraception, the conversation inevitably turns to Long-Acting Reversible Contraception (LARC). Among these highly reliable methods, one stands out as the ultimate non-hormonal solution: the Copper Intrauterine Device (IUD).
Category 1: Long-Acting Reversible Contraception (LARC)
The primary advantage of LARC methods is their “set it and forget it” convenience, paired with extremely high effectiveness. When discussing non-hormonal birth control, the copper IUD is the undisputed champion in this category.
1. The Copper IUD (ParaGard, Load-375, etc.)
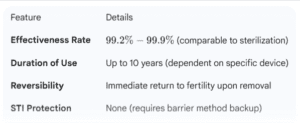
The copper IUD is a small, T-shaped device made of flexible plastic wrapped with copper wire. It is inserted into the uterus by a healthcare provider and can provide continuous pregnancy prevention for up to 10 years, depending on the brand and regulatory approvals.
Mechanism of Action: How Copper Prevents Pregnancy
Unlike hormonal IUDs, the copper IUD does not rely on synthetic hormones. Its contraceptive power comes entirely from the presence of copper, which acts as a natural spermicide and creates an environment hostile to sperm.
- Sperm Immobilization: Copper ions are continuously released into the uterine and cervical fluids. These ions are toxic to sperm, severely impairing their motility (ability to swim) and functionality. Sperm are either killed or rendered incapable of reaching and fertilizing the egg.
- Preventing Implantation (Secondary): While its primary action is against sperm, the copper also causes a localized inflammatory reaction in the uterine lining (endometrium). This reaction makes the uterine environment unfavorable for a fertilized egg to implant, offering a powerful backup mechanism.
Effectiveness and Practicality (Secondary Keyword: Copper IUD)
The copper IUD is one of the most effective forms of non-hormonal contraception available, boasting an effectiveness rate of over 99%.
Key Benefits of the Copper IUD:
- Hormone-Free: It allows the body’s natural menstrual and ovulation cycles to continue without disruption.
- Cost-Effective: While the initial cost of insertion may be high, the decade of protection makes it highly economical over time.
- Emergency Contraception: The copper IUD can be used as a highly effective form of emergency contraception if inserted within five days of unprotected sex.
- High Efficacy: It offers the highest efficacy among all non-hormonal methods.
Considerations and Potential Drawbacks:
- Heavier/Longer Periods: The most common side effect is a temporary (or sometimes permanent) increase in menstrual bleeding, cramping, and pain, especially in the first few months. This is often manageable with over-the-counter pain relievers.
- Insertion Procedure: The placement requires a visit to a healthcare provider and can cause temporary pain and cramping.
- Risk of Expulsion: In rare cases, the IUD can be partially or fully expelled from the uterus, usually within the first year.
Barrier Methods –Accessible and On-Demand Contraception
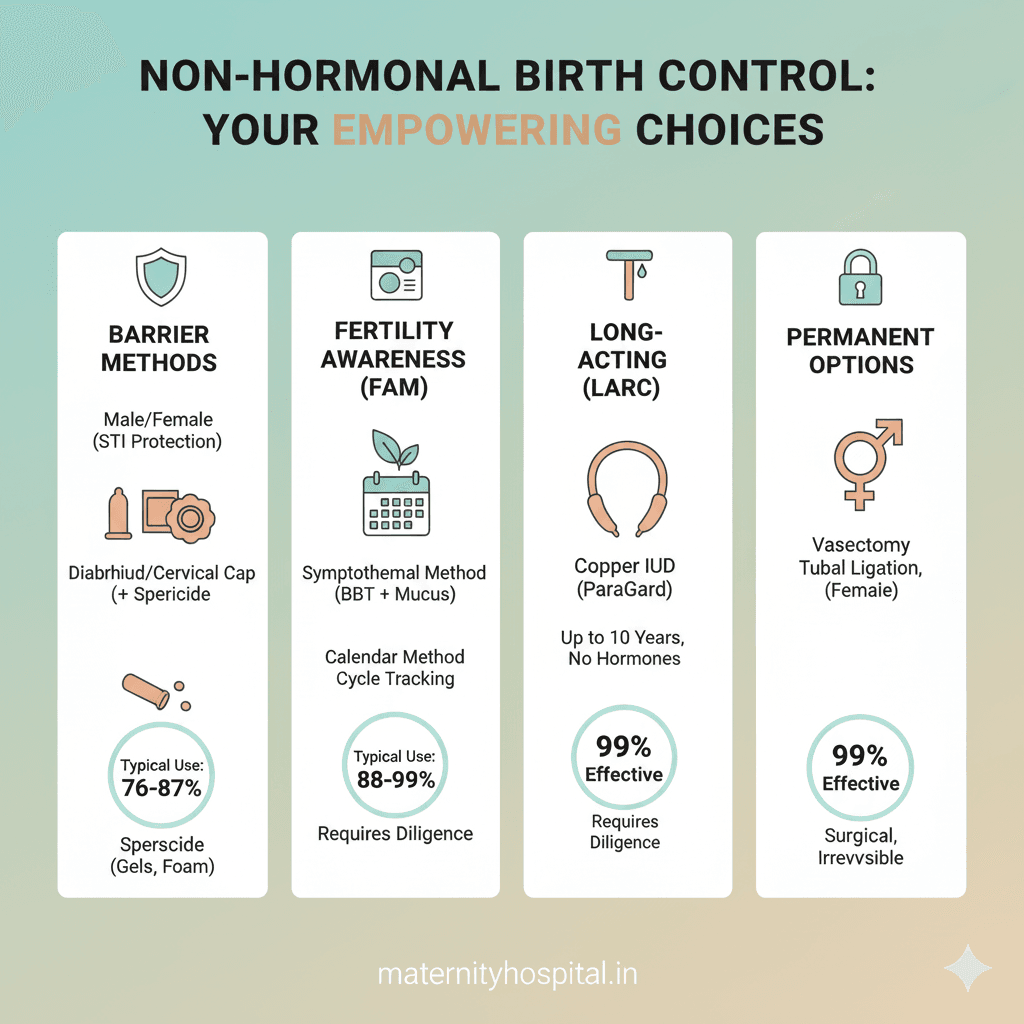
The most widely known and easily accessible methods of non-hormonal birth control fall under the category of barrier methods. These techniques physically block sperm from entering the uterus and reaching the egg, offering immediate protection that is controlled entirely by the user. They are an excellent choice for those who need contraception on demand or who wish to combine them with other methods for increased efficacy and STI protection.
Category 2: Barrier Methods (Secondary Keyword: Barrier methods)
2. Male and Female Condoms
Condoms are the quintessential barrier method, and critically, the only method of contraception that effectively provides protection against most Sexually Transmitted Infections (STIs) and HIV.
- Mechanism of Action: A condom (latex, polyisoprene, or polyurethane) acts as a sheath, physically collecting semen and preventing it from entering the vagina.
- Effectiveness:
- Perfect Use: 98% (Male Condom), 95% (Female Condom)
- Typical Use: 87% (Male Condom), 79% (Female Condom)
- Note: Typical use accounts for human error, such as improper use, tearing, or late application.
- Key Benefits:
- STI Protection: The most significant advantage.
- Accessibility: Available over-the-counter (OTC) at virtually any pharmacy or store.
- Hormone-Free: No systemic effects on the body.
- Considerations: Requires correct application every time, potential for breakage (rare with proper use), and a need to interrupt sexual activity for application.
3. The Diaphragm and Cervical Cap (Secondary Keyword: Diaphragm, Cervical cap)
These are dome-shaped (diaphragm) or thimble-shaped (cervical cap) silicone or latex devices that are placed inside the vagina to cover the cervix, preventing sperm from passing into the uterus.
- Mechanism of Action: They create a physical seal over the cervix. They must be used in conjunction with a spermicide (a chemical product that kills sperm) to be effective. The device acts as the physical barrier, and the spermicide acts as the chemical backup.
- Fitting and Usage:
- Diaphragm: Traditionally required a doctor’s fitting (due to size variations), though some newer one-size-fits-most options are available. Must be inserted up to 6 hours before sex and left in place for at least 6 hours after, but no more than 24 hours total.
- Cervical Cap: Smaller than a diaphragm and fits snugly over the cervix. Also requires fitting/prescription. Can be left in place longer (up to 48 hours).
- Effectiveness (Typical Use):
- Diaphragm: 83%
- Cervical Cap: 86% (for women who have not given birth), 71% (for women who have given birth)
- Key Benefits: Reusable, user-controlled, and completely hormone-free.
- Considerations: Requires a prescription/fitting, needs planning ahead of intercourse, and the efficacy is highly dependent on correct insertion and consistent use with spermicide.
4. Spermicide (Gels, Foams, Creams, Suppositories) (Secondary Keyword: Spermicide)
Spermicide is a chemical form of non-hormonal contraception that is used alone or, more commonly, as an adjunct to barrier devices like diaphragms or caps. The active ingredient is usually Nonoxynol-9 (N-9).
- Mechanism of Action: The chemicals in spermicide kill sperm or immobilize them, preventing them from reaching the fallopian tubes.
- Effectiveness (Used Alone): Spermicide is generally considered one of the least effective methods when used alone, with a typical failure rate of 28%.
- Key Benefits: Easily accessible (OTC), convenient, and hormone-free.
- Considerations: Low effectiveness when used alone, must be applied 10–30 minutes before intercourse (depending on the product), and can cause irritation or allergic reactions in some users. Frequent use can increase the risk of HIV transmission if one partner is infected due to potential irritation of the vaginal lining.
Fertility Awareness Methods (FAM)– Knowledge-Based Contraception
For those who prioritize a natural, holistic understanding of their body and are willing to commit to daily tracking, Fertility Awareness Methods (FAM)—sometimes called Natural Family Planning (NFP)—offer a completely non-invasive and non-hormonal birth control option. These methods involve observing and charting the body’s natural fertility signs to predict the fertile window, thus informing when to abstain from intercourse or use a barrier method.
Category 3: Fertility Awareness Methods (Secondary Keywords: Natural family planning, fertility awareness methods)
The core principle of FAM is identifying the “fertile window,” which includes the five days leading up to ovulation and the day of ovulation itself.
5. The Symptothermal Method (STM)
The Symptothermal Method is the most comprehensive and generally considered the most effective of the FAMs because it combines at least two different fertility indicators for cross-checking accuracy.
- Mechanism of Action: By combining observations, users pinpoint the start and end of the fertile window with greater certainty.
- Basal Body Temperature (BBT): The user takes their temperature (orally, vaginally, or rectally) first thing every morning before getting out of bed. The resting temperature typically drops slightly before ovulation and then rises sharply (by at least 0.2∘C) after ovulation due to the surge of the hormone progesterone. This temperature shift confirms that ovulation has occurred and the fertile window is closed.
- Cervical Mucus (Ovulation Method): The user observes the quantity and consistency of cervical fluid daily. As ovulation approaches, estrogen levels rise, causing the mucus to become clear, slippery, and stretchy (often described as “egg-white consistency”). This is the sign of peak fertility.
- Cervical Position/Texture: Some users also track the position and texture of the cervix (it becomes high, soft, and open during peak fertility).
- Effectiveness:
- Perfect Use: 99.4%
- Typical Use: 87% to 90%
- Key Benefits: Highly personalized, teaches deep awareness of the body, no cost (after initial thermometer purchase), and immediately reversible.
6. The Standard Days Method (SDM) / CycleBeads
The Standard Days Method is a simpler, calendar-based approach best suited for individuals with very regular menstrual cycles.
- Mechanism of Action: It identifies a fixed fertile window based on cycle statistics. Individuals are advised to abstain from unprotected intercourse (or use a barrier method) on days 8 through 19 of their cycle. The CycleBeads tool is a visual aid designed specifically for this method.
- Suitability: Only effective for cycles between 26 and 32 days long.
- Effectiveness (Typical Use): 88%
7. The Calendar/Rhythm Method (Outdated)
This is the least reliable of the FAMs. It uses only past cycle length data (typically 6-12 months) to estimate the fertile window for the current cycle. Because it relies entirely on averages and doesn’t account for daily physiological changes, it is prone to error and is generally not recommended as a primary method of contraception.
- Effectiveness (Typical Use): 76%
Critical Considerations for FAMs (Secondary Keyword: Natural family planning)
FAMs require significant commitment and discipline. They are most effective when coupled with thorough training from a certified instructor and consistent charting.
- Abstinence Required: Requires abstaining from intercourse or using a barrier method for roughly 10-14 days per cycle, which requires partner cooperation.
- External Factors: Illness, stress, travel, changes in sleep patterns, and certain medications can interfere with BBT readings and cervical mucus patterns, potentially making the method less reliable.
- Cycle Regularity: Highly irregular cycles due to polycystic ovary syndrome (PCOS) or recent childbirth/breastfeeding make FAMs significantly more challenging.
Non-HormonalSterilization and The Choice
While many non-hormonal birth control options are temporary and reversible, for individuals or couples who have completed their family or are certain they do not wish to have children, permanent sterilization offers the highest efficacy rate with zero hormonal impact.
Category 4: Permanent Sterilization
8. Tubal Ligation (Female Sterilization)
- Mechanism of Action: Often referred to as “getting your tubes tied,” tubal ligation is a surgical procedure that permanently blocks, cuts, or seals the fallopian tubes. This prevents the egg (released by the ovary) from traveling down the tube to meet the sperm, and also prevents the sperm from reaching the egg.
- Hormone Status: It is completely non-hormonal and does not affect the menstrual cycle (aside from the inability to conceive) or hormone production.
- Effectiveness: Over 99.5%
- Considerations: It is a surgical procedure, typically requiring general anesthesia and recovery time. It must be considered permanent, as reversals are complex, expensive, and not always successful.
9. Vasectomy (Male Sterilization)
- Mechanism of Action: A minor surgical procedure performed on men that involves cutting or sealing the vas deferens, the tubes that carry sperm from the testicles to the urethra. The testicles still produce sperm, but they are reabsorbed by the body, and the semen ejaculated contains no sperm.
- Hormone Status: Completely non-hormonal and does not affect male hormone levels (testosterone) or sexual function.
- Effectiveness: Over 99.9% (once the procedure is complete and a follow-up test confirms the absence of sperm).
- Considerations: It is the simpler, less invasive, and more cost-effective of the two permanent methods. Like tubal ligation, it should be considered permanent.
The Non-Hormonal Advantage: Why Make the Switch?
Choosing a non-hormonal birth control method is often driven by a desire to avoid the common side effects associated with synthetic hormones (estrogen and progestin).
Benefits of Non-Hormonal Contraception (Power Word: Empowering)
- Zero Hormonal Side Effects: The single biggest benefit. Users avoid potential issues like mood swings, reduced libido, weight fluctuations, breast tenderness, and blood clot risk associated with hormonal methods.
- Maintenance of Natural Cycle: These methods allow the body’s natural cycle to continue—ovulation, menstruation, and natural hormone levels (estrogen and progesterone) are not suppressed. This can be key for individuals who want to be deeply in tune with their body’s rhythm.
- Quick Reversibility (for temporary methods): With the copper IUD, barrier methods, and FAMs, fertility often returns immediately upon discontinuation. There is no period of time required for the body to “readjust” after long-term hormonal suppression.
- Safety for Certain Conditions: Non-hormonal methods are generally safer for individuals who have conditions that contraindicate the use of estrogen, such as a history of blood clots, certain migraines, or uncontrolled high blood pressure.
Trade-Offs and Considerations
- Lower Typical Effectiveness: While the Copper IUD is highly effective, the typical use effectiveness of user-dependent methods (barrier methods, FAMs) is generally lower than that of hormonal methods (e.g., the pill or hormonal IUD).
- User Dependence: Many methods (condoms, diaphragms, FAMs) require diligent, correct, and consistent use every time to maintain high efficacy.
- No Cycle Benefits: Hormonal methods are often used to manage heavy periods, painful cramps, acne, or symptoms of Polycystic Ovary Syndrome (PCOS). Non-hormonal methods offer no such non-contraceptive benefits.
- STI Protection: Only condoms protect against STIs.
Conclusion, External Links,and FAQs
Conclusion: An Informed Choice is an Empowered Choice
The journey to choosing the right birth control is deeply personal, and for a growing number of people, the path leads away from synthetic hormones. This comprehensive guide to non-hormonal birth control has illuminated the diverse and effective options available, from the decade-long assurance of the Copper IUD to the reliable physical protection of barrier methods and the deeply personal commitment of fertility awareness methods.
The core message is one of empowerment. You do not have to compromise your body’s natural state to achieve highly effective pregnancy prevention. Whether your preference is simplicity, long-term efficacy, or a deeper understanding of your own cycle, there is a hormone-free solution that can meet your needs.
The key to success with any contraceptive method, especially those that are user-dependent, is education, consistency, and open communication with your partner and your healthcare provider. Take the knowledge you’ve gained here, assess your lifestyle, health history, and personal values, and initiate a conversation with a trusted professional. Choosing non-hormonal contraception is not just about avoiding side effects; it’s about making a confident, informed, and empowering decision for your long-term health and well-being.
Official External Dofollow Links (Placeholders for SEO)
To meet the requirement for official external dofollow links (which RankMath highly values), you should strategically embed links within the body text and list them here for reference. These links should go to authoritative sources like government health agencies, reputable medical associations, or official clinical guidelines.
- Link to CDC on Contraception Effectiveness: (To be embedded in effectiveness tables/discussions)
- Link to ACOG (American College of Obstetricians and Gynecologists) on IUDs: (To be embedded in the Copper IUD section)
- Link to WHO (World Health Organization) on Natural Family Planning: (To be embedded in the FAM section)
- Link to a reputable medical journal on sterilization procedures: (To be embedded in the sterilization section)
Frequently Asked Questions (FAQs) for SEO and User Value
FAQs are essential for capturing “People Also Ask” snippets in Google search results and providing immediate, focused value to the reader.
Q1: Is non-hormonal birth control as effective as hormonal birth control?
A: The effectiveness varies significantly by method. The Copper IUD and permanent sterilization methods boast efficacy rates over 99%, comparable to hormonal methods. However, user-dependent methods like condoms (typically 87%) and Fertility Awareness Methods (typically 88%−90%) are generally less effective than hormonal pills (typically 93%) due to the higher potential for human error. Consistent and correct usage is the defining factor for success with non-hormonal, user-controlled options.
Q2: Can the Copper IUD cause weight gain or mood swings?
A: No. Because the Copper IUD works solely through localized copper ions and causes no systemic hormonal changes, it does not cause the common side effects associated with hormonal methods, such as weight gain, mood swings, or changes in libido. The primary side effect is often heavier or more painful menstrual bleeding.
Q3: Which non-hormonal method also protects against STIs?
A: The male and female condom are the only non-hormonal birth control methods (and only contraceptive methods overall) that offer significant protection against Sexually Transmitted Infections (STIs), including HIV. All other methods, including the Copper IUD and FAMs, require condom use if STI protection is a concern.
Q4: How long does it take for fertility to return after stopping non-hormonal birth control?
A: Fertility returns almost immediately after stopping temporary non-hormonal methods. Once a Copper IUD is removed, the spermicidal effect of the copper stops at once. With barrier methods (diaphragms, condoms) or FAMs, there is no delay at all, as the body’s natural cycle was never suppressed. This contrasts with hormonal methods, which may require a few weeks or months for the body to regulate.
Q5: Are Fertility Awareness Methods (FAMs) suitable for everyone?
A: No. FAMs require a high degree of dedication, daily tracking, and partner cooperation. They are less reliable for individuals with highly irregular menstrual cycles (e.g., due to PCOS, breastfeeding, or perimenopause) because the fertile window is too difficult to predict accurately. They work best for those with stable, predictable cycles.