What Is Ovulation? Timing, Period, and The Core of Your Menstrual Cycle
Introduction –The Central Event of the Female Reproductive Cycle (Expanded)
Last Updated . Designer
For anyone charting their reproductive journey—be it for achieving conception, employing natural family planning, or simply seeking deep physiological self-knowledge—no topic holds more importance than ovulation. It is the non-negotiable event at the heart of the menstrual cycle, determining the possibility of pregnancy.
Many people confuse the broad span of their “menstrual cycle” with the specific, fleeting time known as the “fertile window.” However, ovulation is the single, crucial biological process—the moment the body successfully releases a mature egg—that initiates the short, six-day window when fertilization can occur. Without this successful release, the intricate hormonal cascade that leads to conception simply cannot begin.
If you are currently relying on guesswork, simple calendar apps, or vague assumptions about your cycle, you could be missing your peak fertility days.
WARNING: Your Cycle App Lies. This authoritative, detailed guide is structured to turn vague hopes into precise knowledge. Drawing on definitions and timings from leading medical bodies, we will dissect:
- What is ovulation in scientific terms.
- Precisely what is the ovulation period and the crucial fertile window.
- The profound connection between ovulation and menstruation.
- The life-long timeline: when ovulation starts and ends in which age range.
Mastering this subject empowers you to take absolute control of your body’s most fundamental biological rhythm, transforming uncertainty into proactive, confident reproductive planning.
The Core Mechanics:What is Ovulation? The Biological Definition (Deep Dive)
To truly understand your fertility, you must look past simple day counting and appreciate the complex biology that orchestrates the release of the ovum. Ovulation is defined as the phase in the menstrual cycle when a mature, dominant ovarian follicle ruptures, expelling the oocyte (egg) into the fallopian tube [Source: Clue App, citing ACOG principles]. This biological event is the zenith of the follicular phase and the prelude to the secretory phase.
The Hypothalamic-Pituitary-Ovarian (HPO) Axis: The Master Clock
Ovulation is an elaborate hormonal performance, conducted by the brain’s hypothalamus and pituitary gland, and the ovaries themselves. This control system, the HPO Axis, works on precise positive and negative feedback loops.
1. The Follicular Phase: Maturation and Proliferation
The cycle begins (Day 1) with the commencement of menses, but the follicular phase is already underway. This phase is characterized by:
- FSH Stimulation: The hypothalamus signals the pituitary gland to release Follicle-Stimulating Hormone (FSH). FSH acts on the ovaries, prompting approximately 15–20 primordial follicles to begin maturing. This process is highly competitive; typically, only one follicle, the dominant follicle, will reach full maturity.
- Estrogen Surge (Positive Feedback): As the dominant follicle grows, it becomes a prolific producer of estrogen (specifically 17-β estradiol). This estrogen has two vital roles:
Uterine Preparation: It signals the endometrial lining to thicken and proliferate, building a rich, vascular bed for potential implantation.
The Switch: When estrogen levels cross a critical threshold, it stops providing negative feedback and initiates a massive surge of positive feedback to the pituitary gland.
2. The LH Surge: The Unavoidable Trigger
The positive feedback from high estrogen levels causes the pituitary to release an explosive amount of Luteinizing Hormone (LH)—the LH Surge.
- Timing: The LH surge typically begins 34–36 hours before the follicle ruptures, making it a highly reliable predictor of the ovulation time.
- Action: LH triggers a cascade of internal cellular and enzymatic changes within the dominant follicle, including the production of prostaglandins and proteolytic enzymes. These enzymes digest the collagen structure of the follicular wall, leading to the formation of a weak spot known as the stigma.
- The Ejection: The high fluid pressure within the follicle, combined with the structural weakening, results in the explosive release of the ovum-cumulus complex (the egg surrounded by protective cells) from the ovary’s surface. This is the moment of ovulation.
The egg, now in the peritoneal cavity, is quickly captured by the finger-like projections (fimbriae) of the fallopian tube, where its journey toward the uterus begins.
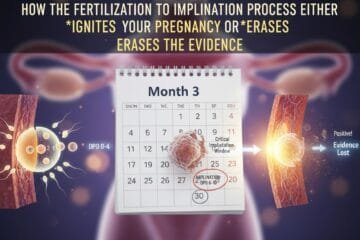
What is the Ovulation Period and Fertile Window?Precision Timing for Conception
When tracking fertility, it is crucial to distinguish between the lifespan of the egg and the lifespan of the sperm, as their overlap determines your actual chances of pregnancy.
The Single-Day Ovulation Period
The ovulation period is startlingly brief. Once the egg is released:
- Fertilization Clock: The egg remains viable for fertilization for a maximum of 12 to 24 hours [Source: Mayo Clinic]. After this window, the ovum rapidly degrades, and the opportunity for conception in that cycle ends.
This short timeframe is why solely timing intercourse after confirming ovulation (e.g., after the BBT rise) is often too late.
The Multi-Day Fertile Window: Maximizing Opportunity
The fertile window leverages the survival time of sperm, which is significantly longer than the egg’s.
- Sperm Survival: Sperm, protected by the nutrient-rich, egg-white-like cervical mucus (discussed below), can survive within the female reproductive tract for up to five days
- The Six-Day Span: Therefore, the fertile window is calculated as the six-day period ending on the day of ovulation (5 days prior to ovulation + the day of ovulation itself). This ensures that live, viable sperm are waiting in the fallopian tube when the egg is finally released.
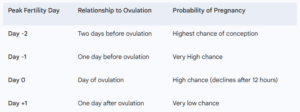
Conclusion on Timing: For individuals seeking pregnancy, the most effective strategy is to have intercourse every day or every other day during the 3-day peak (Day -2, Day -1, and Day 0).
Methods for Determining Ovulation Time
Pinpointing the exact ovulation time requires triangulation using multiple fertility awareness methods (FAMs):
1. Luteinizing Hormone (LH) Testing
- What it is: Over-the-counter Ovulation Predictor Kits (OPKs) measure the LH concentration in urine.
- What it indicates: A positive test confirms the LH surge is occurring, predicting ovulation will happen in the next 24–36 hours. This is the best tool for forward prediction.
2. Cervical Mucus Monitoring (The Real-Time Signal)
- What it is: Changes in the fluid secreted by the cervix throughout the cycle.
- What it indicates: Just before and during peak fertility, estrogen causes the mucus to become thin, clear, highly stretchy, and slippery, resembling raw egg whites (EWCM). This mucus is essential for sperm mobility and survival. The presence of EWCM is the strongest real-time indicator that the fertile window is open.
3. Basal Body Temperature (BBT) Charting
- What it is: Measuring the body’s lowest resting temperature upon waking, before any activity.
- What it indicates: The production of progesterone (by the Corpus Luteum after ovulation) is thermogenic, causing a sustained temperature jump of 0.5 to 1.3∘F (0.3 to 0.7∘C) . BBT charting is the method used to retrospectively confirm that ovulation has occurred, signaling the fertile window has closed for that cycle.
What is Ovulation and Menstruation?The Hormonal Relationship
Ovulation and menstruation are inextricably linked, representing two endpoints of the same cycle. Think of the menstrual cycle as a grand performance where ovulation is the climax, and menstruation is the curtain call if the audience (a fertilized egg) doesn’t appear.
The entire 21– to 35-day cycle can be divided into the Ovarian Cycle (what happens in the ovary) and the Endometrial Cycle (what happens in the uterus), which align perfectly.
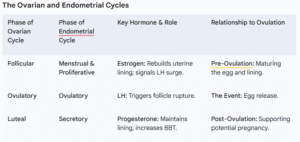
Menstruation: The Default Reset
The transition from the Luteal phase back to Menstruation (Day 1) is the core failure mechanism of a non-pregnant cycle:
- After ovulation, the ruptured follicle transforms into the Corpus Luteum.
- The Corpus Luteum produces high levels of progesterone and some estrogen, which stabilize and enrich the uterine lining, making it receptive to a blastocyst.
- If no fertilization and subsequent implantation of an embryo occur within approximately 12−14 days, the Corpus Luteum automatically begins to degrade (luteolysis).
- The immediate, dramatic drop in circulating progesterone and estrogen levels triggers vasoconstriction and tissue breakdown in the uterine lining. This shedding process is menstruation.
The Key Takeaway: The length of time between ovulation and the start of the next period (the luteal phase) is remarkably consistent for most people, averaging 14 days. It is the phase before ovulation (the follicular phase) that accounts for most of the variation in cycle length (e.g., a 21-day cycle has a 7-day follicular phase; a 35-day cycle has a 21-day follicular phase).
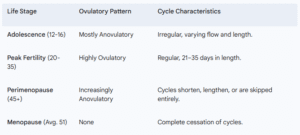
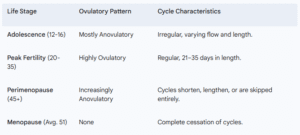
When Ovulation Starts and Ends in Which Age?The Reproductive Lifespan
Ovulation capacity defines the total reproductive window, which is governed by the finite supply of ovarian follicles present from birth.
The Start: Menarche and the First Cycles
Ovulation is conceptually linked to the first menstrual period, but the reality is more nuanced.
Menarche (First Period)
- Average Onset: The first menstrual period, or Menarche, typically occurs around age 12 years, although the normal range extends from 10 to 16.
- The Lag Period: The onset of menarche merely indicates the HPO axis is waking up. For the first 1–2 years following menarche, menstrual cycles are often anovulatory (bleeding without egg release) and irregular. The axis is still immature, and the necessary LH surges may not be strong enough or timely enough to trigger ovulation.
- When Regular Ovulation Begins: It may take up to three to five years for a stable, adult pattern of regular, ovulatory cycles to establish. The ability to ovulate consistently is typically well-established by the late teens and early twenties.
The Peak and Decline: Mid-Adulthood and Age 35
The mid-reproductive years are characterized by highly regular, predictable ovulation, which provides the highest probability of conception.
- Age 20s to Early 30s: Peak fertility years, where the vast majority of cycles are ovulatory, and the quality of the eggs is highest.
- Age 35 (The Benchmark): Reproductive aging accelerates significantly around age 35. While ovulation continues, the follicle quality declines, and the overall ovarian reserve begins to drop at a steeper rate. Furthermore, the follicular phase tends to shorten with age (e.g., from 14 days in the 20s to potentially 10 days in the 40s). A shorter follicular phase means periods come closer together, but the luteal phase remains fixed.
The End: Perimenopause and Menopause
The ability to ovulate ceases when the supply of viable follicles is functionally depleted, signaling the end of reproductive life.
Perimenopause (The Transition)
- Timing: Often begins in the mid-to-late 40s, lasting an average of 4 years.
- Irregularity: Hormonal production becomes erratic. LH surges may fail to occur, or multiple follicles may be attempted. Anovulatory cycles becomes common, leading to irregular, skipped, or very light/heavy periods. Ovulation is still possible, but unpredictable.
Menopause (The Cessation)
- Diagnosis: Defined retrospectively after 12 consecutive months without a menstrual period.
- Average Age: The average age of menopause in industrialized countries is approximately 51 years. After menopause, no viable follicles remain, and ovulation ceases permanently.
Ovulation Irregularities, Anovulation and When to Seek Help
The complexity of the HPO axis means that disruptions—from minor lifestyle changes to underlying medical conditions—can halt the process of ovulation, a condition known as anovulation.
Common Causes of Anovulation
Anovulation is the leading cause of infertility and highly irregular cycles. Understanding the root cause is the first step toward treatment:
- Polycystic Ovary Syndrome (PCOS): This endocrine disorder interferes with the hormonal balance (LH, FSH, testosterone), preventing the dominant follicle from maturing and rupturing, leaving a string of small, undeveloped cysts on the ovary.
- Thyroid Disease: Both an underactive (hypo) or overactive (hyper) thyroid can create hormone imbalances that directly disrupt the HPO axis and suppress ovulation.
- Stress and Weight: Significant or prolonged physical or emotional stress, along with rapid or extreme weight fluctuations (low BMI or obesity), can disrupt the communication between the hypothalamus and the pituitary, effectively putting the reproductive system on hold. This is known as hypothalamic amenorrhea.
- Hyperprolactinemia: An excess of the hormone prolactin (often related to pituitary issues) can suppress the pulsatile release of GnRH, preventing the necessary FSH and LH production.
- Perimenopause: As mentioned, anovulation becomes a natural, expected part of the transition leading up to menopause as the ovarian reserve diminishes.
When to Consult a Specialist
If you are tracking your cycle and consistently noticing signs of anovulation (no LH surge, no BBT rise, consistently dry cervical mucus), or if your cycle is highly irregular, medical consultation is warranted.
- Age Under 35: Consult a fertility specialist if you have been trying to conceive for 12 months or more without success.
- Age 35 or Older: Consult a specialist if you have been trying to conceive for 6 months or more without success.
Medical interventions often involve simple diagnostic tests (blood hormone levels, ultrasound) and treatments like oral medications (e.g., Clomiphene Citrate) to stimulate the ovaries and induce the necessary hormonal surge for ovulation.
Conclusion: The Power of Knowing Your Cycle
Ovulation is more than just a biological detail; it is the ultimate expression of the body’s reproductive vitality. By moving from a passive understanding of “getting a period” to an active, precise tracking of the ovulation period and fertile window, you transition from being a passenger to the driver of your reproductive health.
You now possess the authoritative knowledge to answer what is ovulation, how it dictates your period, and the age-related shifts across your lifespan. Use this knowledge to Master Your Fertility and instead, unlock a clearer, more powerful path to fertility and bodily awareness. Always partner this awareness with guidance from a trusted medical professional for personalized care.
Frequently Asked Questions (FAQs)
Q1: How long does the egg live after ovulation? A: The egg has a critical, brief lifespan of only 12 to 24 hours after its release. Beyond this window, it is no longer capable of being fertilized.
Q2: What is the difference between the “ovulation period” and the “fertile window”? A: The ovulation period (egg viability) is 12–24 hours. The fertile window is the larger, six-day span that includes the 5 days before ovulation and the day of ovulation itself, designed to account for the longer survival of sperm (up to 5 days).
Q3: Can I get my period if I don’t ovulate? A: Yes, this is known as an anovulatory cycle. Hormonal fluctuations (specifically the buildup and subsequent slow decline of estrogen) can cause the uterine lining to shed, mimicking a period, even though no egg was released and no corpus luteum was formed.
Q4: Is ovulation always on Day 14? A: No. Ovulation consistently occurs approximately 14 days before the start of your next menstrual period. Therefore, if you have a 30-day cycle, you will ovulate around Day 16. If your cycle is 25 days, you will ovulate around Day 11.
Q5: What is Mittelschmerz? A: Mittelschmerz is a sharp, sometimes dull, unilateral (one-sided) pain felt by some women in the lower abdomen near the time of ovulation. It is harmless and thought to be caused by the follicular fluid or blood released from the ruptured follicle irritating the pelvic lining.
Q6: Does stress affect my ovulation time? A: Yes. Extreme physical or emotional stress can disrupt the hypothalamus, delaying or entirely suppressing the LH surge necessary for ovulation. This lengthens the follicular phase, causing your period to be late or skipped entirely.
Official External Links for Citation
- American College of Obstetricians and Gynecologists (ACOG) – https://www.acog.org/womens-health/faqs/how-to-prepare-for-pregnancy
- National Institutes of Health (NIH) / NCBI Bookshelf (Endotext) – https://www.ncbi.nlm.nih.gov/books/NBK279054/